So there are two types of "code blue" at this hospital:
- MET, which is a true medical emergency (Medical Emergency, True???)
- ART (I have no idea what this stands for) which is not a medical emergency. We, the code team, do not have to respond to them.
On a recent code, I was paged "CODE BLUE: MET, PARKING LOT 5." Part of me wondered if this shouldn't be an ART...was there really a nurse around to determine that this patient's heart had stopped? But then glamorous images of me intubating the patient in the middle of the parking lot on this sunny cold day compelled me to hurry downstairs.
After consulting a map of the hospital campus, I determined which one was parking lot five and jogged over to the adjacent professional building. There, in a stairwell, an elderly man had tripped and fallen. He had a couple lacerations on his forehead, but a passerby had stopped and given him a napkin. I quickly made sure the bleeding was controlled and did a brief neurological assessment. He was fine. It should have been an ART. Actually, they should have just called 911 rather then going through the hospital pager system.
The code at 7:45 AM the following call day was a little more legitimate. I had decided to take a quick nap after seeing my ICU patient. (Since the team on call the day before my team only has one intern, my call room goes unused, and is ready for napping virtually the moment I arrive.) Being awakened by my pager, I stumbled downstairs to the eighth floor and met my resident in the stairwell. There were a few nurses in the room, but that was it. Since the respiratory therapist hadn't arrived yet, I dug through the "crash cart" and found an appropriate laryngoscope and endotracheal tube.
We did the usual thing: chest compressions, a few medicines. Intubating the patient was surprisingly easy, given that he was such a large man. I always feel much more comfortable in codes once we have an airway, and I'm not sure if it's because I'm a budding anesthesiologist, or if others feel the same way too. A few people congratulated me on the smooth intubation, which made me feel a little guilty because it was so easy...but sometimes it's best just to accept the compliment.
The rest of the code wasn't so smooth...four times we got a pulseless ventricular tachycardia which meant four shocks with the defibrillator, each one bringing back a regular rhythm at least temporarily. In the meantime, he got bicarbonate, calcium, lidocaine, vasopressin, multiple doses of epinephrine, and two boluses of amiodarone. Finally after thirty minutes, we were still in pulseless v tach. My resident "called" the code, that is to say, we had done everything we could do, and it was time to stop.
Like a machine being powered-down, the room quickly grew quiet: the humming faded, the activity stilled, the oxygen flow was cut off. And then, much to our amazement, the patient's jaw moved--he was trying to breathe! And then, slowly, his right arm lifted off the bed! "Uh, resume compressions!" my resident ordered.
Shortly after this point, the cardiologist showed up. His first question was how long we'd been coding the patient. Thirty minutes. "Have you thought about calling the code?" was his second question! When we explained what had happened, the cardiologist tried a couple shocks with the manual paddles (like you see on TV) rather than the sticker pads. Maybe the cardiologist believed the extra pressure would do some good....maybe he did it just for style points.
In the meantime, both of the patient's arms were rising. Given that the unfortunate guy didn't have a perfusing rhythm, the cardiologist informed us he was simply "posturing", that is, having involuntary muscular reflexes. We decided to try one last shock and one last amiodarone bolus. (Even though one amiodarone bolus is usually sufficient, this would be this patient's third.) Wouldn't you know, that did the trick! He had a pulse and a blood pressure after a grueling 45-minute code. We wheeled him to the ICU (rather than discharge him, as the primary team had been planning to do that day) and let the specialists take over from there.
As if that weren't enough about this remarkable code, the story doesn't end there...by the following afternoon, the patient was ready to be extubated! Evidently he's had full--and rapid--recovery with no neurological deficits after being dead for the better part of an hour!
I also learned a lesson about napping. Right after I'd intubated the patient, my resident turned to me and asked, "Jonathan, were you asleep in the call room? There's a line on your face!" (The lesson is to sleep on my back during my daytime naps.)














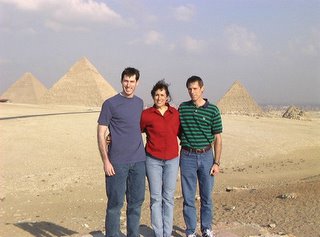


 In Luxor, waiting to travel back to Cairo.
In Luxor, waiting to travel back to Cairo. 






