 Days like today make me glad I have a blog--an avenue to write down thoughts. It started as a way for family and friends to keep up with what I do, as well as for me to remember fun or interesting things in life. Another secondary purpose which developed is simply to entertain people (even strangers) with interesting stories. However, today I take advantage of writing as a way to reflect.
Days like today make me glad I have a blog--an avenue to write down thoughts. It started as a way for family and friends to keep up with what I do, as well as for me to remember fun or interesting things in life. Another secondary purpose which developed is simply to entertain people (even strangers) with interesting stories. However, today I take advantage of writing as a way to reflect.In a previous post entitled I hate this part of the job, I recognized how difficult it is to break bad news to a patient. Today, however, I deal with the fact that I AM bad news to the patient. At least I can be.
It all began when I walked into the residents' lounge today. The resident on call informed me a patient I'd discharged on Saturday was back--with angioedema, a life-threatening condition. Angioedema is swelling in non-dependent places; in other words, swelling not affected by gravity. I generally think of it as an allergic/immune response, and it's dangerous because the airway can swell, essentially suffocating the patient.
In the ABC's of medical emergencies, the A is for airway. It's the most essential thing for maintaining that fragile balance we call life. In this patient with a recent heart attack, the admitting team was reluctant to use epinephrine to counteract the angioedema because it could stimulate the heart and precipatate another massive heart attack. Fiberoptic nasotracheal intubation was attempted in the emergency department, with the result that the patient developed a life-threatening cardiac arrhythmia. She was eventually stabilized and brought to the ICU, where she remains.
The problem began a week or so ago. This pleasant 80-something patient had a list of 10 medicines she took, and 10 she was allergic to. One of the meds, labeled by its proper name, I jotted down with the comment, "face swelling." I wasn't familiar with the name of the medicine (not too uncommon a situation, as there are many thousands of medicines), but I didn't take the time to look it up.
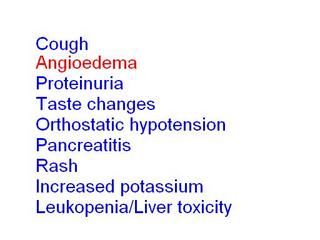
To make an unfortunate story short, we started her on an ACE-inhibitor, a great blood pressure medicine, which just so happened to be one of the two drugs in the name of the tablet I wrote down on my admitting H&P. While there were multiple layers of protection against this sort of thing that should have been in place (my attending, my resident, the pharmacy--which knew of her allergy), the fact is that I was practicing medicine and I neglected to investigate a key piece of information, to this patient's detriment. She was on this medicine for several days before discharge, but the side effect began the day after going home. (The graphic at the top has a mnemonic we learned as second-year medical students with the side effects of ACE-inhibitors.)
I can't help but remember some of the last words she spoke to me before I discharged her, "Thank you for taking such good care of me!" Little did she know we were poisoning her. She didn't have the medical training. We did.
I don't know what will become of this situation in the legal sense (and hence it may not be the wisest to post this entry), but I know that I have a much greater respect for the power of medicines, both to heal and to harm. And my prayer is that she survives this second hospitalization without a permanent mark on her life of my mistake.






3 comments:
Sorry about the situation, Jonathan. I hope everything turns out all right. I'm proud of you for being so forthright about your mistake, but I hope you don't get bogged down by guilt like I so often do. We're human and we make mistakes, and I'm sure you'll have to remind me of that one of these days.
I almost did exactly the same thing to one of my patients a few months ago, but the pharmacy caught it and called me. All the more worse because it was his only allergy, and I was the one who originally documented it on his chart....Doh!!
Dude, that stinks man. Have you spoken to the patient and the family about the mistake yet?
Post a Comment